Amoxicillin Allergy: Old Concepts, New Concepts and Change of Concepts
DOI:
https://doi.org/10.58931/cait.2021.1219Abstract
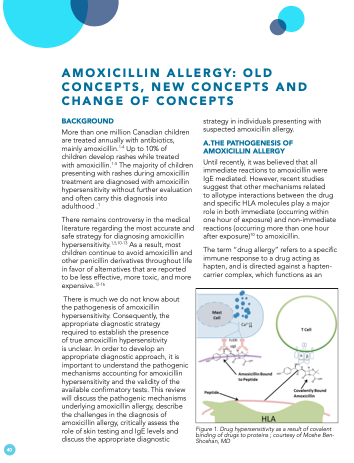
More than one million Canadian children are treated annually with antibiotics, mainly amoxicillin.1-4 Up to 10% of children develop rashes while treated with amoxicillin.1-5 The majority of children presenting with rashes during amoxicillin treatment are diagnosed with amoxicillin hypersensitivity without further evaluation and often carry this diagnosis into adulthood. There remains controversy in the medical literature regarding the most accurate and safe strategy for diagnosing amoxicillin hypersensitivity. As a result, most children continue to avoid amoxicillin and other penicillin derivatives throughout life in favor of alternatives that are reported to be less effective, more toxic, and more expensive. There is much we do not know about the pathogenesis of amoxicillin hypersensitivity. Consequently, the appropriate diagnostic strategy required to establish the presence of true amoxicillin hypersensitivity is unclear. In order to develop an appropriate diagnostic approach, it is important to understand the pathogenic mechanisms accounting for amoxicillin hypersensitivity and the validity of the available confirmatory tests. This review will discuss the pathogenic mechanisms underlying amoxicillin allergy, describe the challenges in the diagnosis of amoxicillin allergy, critically assess the role of skin testing and IgE levels and discuss the appropriate diagnostic strategy in individuals presenting with suspected amoxicillin allergy.
References
Seitz CS, Brocker EB, Trautmann A. Diagnosis of drug hypersensitivity in children and adolescents: discrepancy between physician-based assessment and results of testing. Pediatr Allergy Immunol. 2011 Jun;22(4):405-10. doi:10.1111/j.1399-3038.2011.01134.x
Sidell D, Shapiro NL, Bhattacharyya N. Demographic Influences on Antibiotic Prescribing for Pediatric Acute Otitis Media. Otolaryngol Head Neck Surg. 2012 Apr;146(4):653-8. doi:10.1177/0194599811431228
Vergison A, Dagan R, Arguedas A, Bonhoeffer J, Cohen R, Dhooge I, et al. Otitis media and its consequences: beyond the earache. Lancet Infect Dis. 2010 Mar;10(3):195-203. doi:10.1016/S1473-3099(10)70012-8
Venekamp RP, Sanders SL, Glasziou PP, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2015 Jun 23;2015(6):CD000219. doi:10.1002/14651858.CD000219.pub4
Mill C, Primeau MN, Medoff E, Lejtenyi C, O'Keefe A, netchiporouk E, et al. Assessing the Diagnostic Properties of a Graded Oral Provocation Challenge for the Diagnosis of Immediate and Nonimmediate Reactions to Amoxicillin in Children. JAMA Pediatr. 2016 Jun 6;170(6):e160033. doi:10.1001/jamapediatrics.2016.0033
Satta G, Hill V, Lanzman M, Balakrishnan I. Beta-lactam allergy: clinical implications and costs. Clin Mol Allergy. 2013 Nov 27;11(1):2. doi:10.1186/1476-7961-11-2
Mattingly TJ, 2nd, Fulton A, Lumish RA, et al. The Cost of Self-Reported Penicillin Allergy: A Systematic Review. J Allergy Clin Immunol Pract. 2018 Sep-Oct;6(5):1649-1654 e4. doi:10.1016/j.jaip.2017.12.033
MacLaughlin EJ, Saseen JJ, Malone DC. Costs of beta-lactam allergies: selection and costs of antibiotics for patients with a reported beta-lactam allergy. Arch Fam Med. 2000 Aug;9(8):722-726. doi:10.1001/archfami.9.8.722
Kraemer MJ, Caprye-Boos H, Berman HS. Increased use of medical services and antibiotics by children who claim a prior penicillin sensitivity. West J Med. 1987 Jun;146(6):697-700.
Jeimy S, Ben-Shoshan M, Abrams EM, Ellis AK, Connors L, Wong T. Practical guide for evaluation and management of beta-lactam allergy: position statement from the Canadian Society of Allergy and Clinical Immunology. Allergy Asthma Clin Immunol. 2020 Nov;16(1):95. doi:10.1186/s13223-020-00494-2
MacFadden DR, LaDelfa A, Leen J, et al. Impact of Reported Beta-Lactam Allergy on Inpatient Outcomes: A Multicenter Prospective Cohort Study. Clin Infect Dis. 2016 Oct 1;63(7):904-910. doi:10.1093/cid/ciw462
Abrams E, Netchiporouk E, Miedzybrodzki B, Ben-Shoshan M. Antibiotic Allergy in Children: More than Just a Label. Int Arch Allergy Immunol. 2019;180(2):103-112. doi:10.1159/000501518
Abrams EM, Ben-Shoshan M. Should testing be initiated prior to amoxicillin challenge in children? Clin Exp Allergy. 2019 Aug;49(8):1060-1066. doi:10.1111/cea.13443
Soumelis V, Reche PA, Kanzler H, Yuan W, Edward G, Homey B, et al. Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP. Nat Immunol. 2002 Jul;3(7):673-680. doi:10.1038/ni805
Martinez JA, Ruthazer R, Hansjosten K, Barefoot L, Snydman DR. Role of environmental contamination as a risk factor for acquisition of vancomycin-resistant enterococci in patients treated in a medical intensive care unit. Arch Intern Med. 2003 Sep 8;163(16):1905-1912. doi:10.1001/archinte.163.16.1905
Pepin J, Saheb N, Coulombe MA, Alary M-E, Corriveau M-P, Authier S, et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis. 2005 Nov 1;41(9):1254-1260. doi:10.1086/496986
Illing PT, Mifsud NA, Purcell AW. Allotype specific interactions of drugs and HLA molecules in hypersensitivity reactions. Curr Opin Immunol. 2016 Oct;42:31-40. doi:10.1016/j.coi.2016.05.003
Pichler WJ. Immune pathomechanism and classification of drug hypersensitivity. Allergy. 2019 Aug;74(8):1457-1471. doi:10.1111/all.13765
Adam J, Pichler WJ, Yerly D. Delayed drug hypersensitivity: models of T-cell stimulation. Br J Clin Pharmacol. 2011 May;71(5):701-707. doi:10.1111/j.1365-2125.2010.03764.x
Stekler J, Maenza J, Stevens C, Holte S, Malhotra U, McElrath MJ, et al. Abacavir hypersensitivity reaction in primary HIV infection. AIDS. 2006 Jun 12;20(9):1269-1274. doi:10.1097/01.aids.0000232234.19006.a2
Nicoletti P, Carr DF, Barrett S, McEvoy L, Friedmann PSm, Shear NH, et al. Beta-lactam-induced immediate hypersensitivity reactions: A genome-wide association study of a deeply phenotyped cohort. J Allergy Clin Immunol. 2021 May;147(5):1830-1837.e15. doi:10.1016/j.jaci.2020.10.004
Delli Colli L, Gabrielli S, Abrams EM, O'Keefe A, Protudjer JLP, Lavine E, et al. Differentiating between beta-Lactam-Induced Serum Sickness-Like Reactions and Viral Exanthem in Children Using a Graded Oral Challenge. J Allergy Clin Immunol Pract. 2021 Feb;9(2):916-921. doi:10.1016/j.jaip.2020.08.047
Vyles D, Chiu A, Simpson P, Nimmer M, Adams J, Brousseau DC. Parent-Reported Penicillin Allergy Symptoms in the Pediatric Emergency Department. Acad Pediatr. 2017 Apr;17(3):251-255. doi:10.1016/j.acap.2016.11.004
Mathur AN, Mathes EF. Urticaria mimickers in children. Dermatol Ther. 2013 Nov-Dec;26(6):467-475. doi:10.1111/dth.12103
Starnes L, Patel T, Skinner RB. Urticaria multiforme–a case report. Pediatr Dermatol. 2011 Jul-Aug;28(4):436-438. doi:10.1111/j.1525-1470.2011.01311.x
Sampson HA, Munoz-Furlong A, Campbell RL, Franklin Adkinson Jr N, Allan Bock S, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report–second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006 Apr;47(4):373-380. doi:10.1016/j.annemergmed.2006.01.018
Gabrielli S, Clarke AE, Eisman H, Morris J, Joseph L, La Vieille S, et al. Disparities in rate, triggers, and management in pediatric and adult cases of suspected drug-induced anaphylaxis in Canada. Immun Inflamm Dis. 2018 Mar;6(1):3-12. doi:10.1002/iid3.201
Rodriguez-Martin S, Martin-Merino E, Lerma V, Rodriguez-Miguel A, Gonzalez O, Gonzalez-Herrada C, et al. Incidence of Stevens-Johnson syndrome/toxic epidermal necrolysis among new users of different individual drugs in a European population: a case-population study. Eur J Clin Pharmacol. 2019 Feb;75(2):237-246. doi:10.1007/s00228-018-2569-3
Belver MT, Michavila A, Bobolea I, et al. Severe delayed skin reactions related to drugs in the paediatric age group: A review of the subject by way of three cases (Stevens-Johnson syndrome, toxic epidermal necrolysis and DRESS). Allergol Immunopathol (Madr). 2016 Jan-Feb;44(1):83-95. doi:10.1016/j.aller.2015.02.004
Lee P, Shanson D. Results of a UK survey of fatal anaphylaxis after oral amoxicillin. J Antimicrob Chemother. 2007 Nov;60(5):1172-1173.
Schlosser KA, Maloney SR, Horton JM, et al. The association of penicillin allergy with outcomes after open ventral hernia repair. Surg Endosc. 2020 Sep;34(9):4148-4156. doi:10.1007/s00464-019-07183-1
Li PH, Siew LQC, Thomas I, et al. Beta-lactam allergy in Chinese patients and factors predicting genuine allergy. World Allergy Organ J. 2019 Sep 16;12(8):100048. doi:10.1016/j.waojou.2019.100048
Liang EH, Chen LH, Macy E. Adverse reactions associated with penicillins, carbapenems, monobactams, and clindamycin: A retrospective population-based study. J Allergy Clin Immunol Pract. 2020 Apr;8(4):1302-1313.e2. doi:10.1016/j.jaip.2019.11.035
Thompson DF, Ramos CL. Antibiotic-Induced Rash in Patients With Infectious Mononucleosis. Ann Pharmacother. 2017 Feb;51(2):154-162. doi:10.1177/1060028016669525
Leon G. Epidemiology. Vol 4 Philadelphia: Saunders; 2009.
Ibanez MD, Rodriguez Del Rio P, Lasa EM, Joral A, Ruiz-Hornillos J, Munoz C, et al. Prospective assessment of diagnostic tests for pediatric penicillin allergy: From clinical history to challenge tests. Ann Allergy Asthma Immunol. 2018 Aug;121(2):235-244.e3. doi:10.1016/j.anai.2018.05.013
Tannert LK, Mortz CG, Skov PS, Bindslev-Jensen C. Positive Skin Test or Specific IgE to Penicillin Does Not Reliably Predict Penicillin Allergy. J Allergy Clin Immunol Pract. 2017 May-Jun;5(3):676-683. doi:10.1016/j.jaip.2017.03.014
Caubet JC, Eigenmann PA. Managing possible antibiotic allergy in children. Curr Opin Infect Dis. 2012 Jun;25(3):279-85. doi:10.1097/QCO.0b013e3283523f8b
Hjortlund J, Mortz CG, Skov PS, Bindslev-Jensen C. Diagnosis of penicillin allergy revisited: the value of case history, skin testing, specific IgE and prolonged challenge. Allergy. 2013 Aug;68(8):1057-1064. doi:10.1111/all.12195
Moral L, Caubet JC. Oral challenge without skin tests in children with non-severe beta-lactam hypersensitivity: Time to change the paradigm? Pediatr Allergy Immunol. 2017 Dec;28(8):724-727. doi:10.1111/pai.12800
Solensky R, Jacobs J, Lester M, Lieberman P, McCafferty F, Nilsson T, et al. Penicillin Allergy Evaluation: A Prospective, Multicenter, Open-Label Evaluation of a Comprehensive Penicillin Skin Test Kit. J Allergy Clin Immunol Pract. 2019 Jul-Aug;7(6):1876-1885 e1873. doi:10.1016/j.jaip.2019.02.040
Loong TW. Understanding sensitivity and specificity with the right side of the brain. BMJ. 2003 Sep;327(7417):716-719. doi:10.1136/bmj.327.7417.716
Harandian F, Pham D, Ben-Shoshan M. Positive penicillin allergy testing results: a systematic review and meta-analysis of papers published from 2010 through 2015. Postgrad Med. 2016 Aug;128(6):557-562. doi:10.1080/00325481.2016.1191319
Marrs T, Fox AT, Lack G, du Toit G. The diagnosis and management of antibiotic allergy in children: Systematic review to inform a contemporary approach. Arch Dis Child. 2015 Jun;100(6):583-588. doi:10.1136/archdischild-2014-306280
Shenoy ES, Macy E, Rowe T, Blumenthal KG. Evaluation and Management of Penicillin Allergy: A Review. JAMA. 2019 Jan 15;321(2):188-199. doi:10.1001/jama.2018.19283
Mori F, Cianferoni A, Barni S, Pucci N, Rossi ME, Novembre E. Amoxicillin allergy in children: five-day drug provocation test in the diagnosis of nonimmediate reactions. J Allergy Clin Immunol Pract. 2015 May-Jun;3(3):375-380.e371. doi:10.1016/j.jaip.2014.11.001
Frieri M, Kumar K, Boutin A. Antibiotic resistance. J Infect Public Health. 2017 Jul-Aug;10(4):369-378. doi:10.1016/j.jiph.2016.08.007
Van Gasse AL, Ebo DG, Chiriac AM, Hagendorens MM, Faber MA, Coenen S, et al. The Limited Value of Prolonged Drug Challenges in Nonimmediate Amoxicillin (Clavulanic Acid) Hypersensitivity. J Allergy Clin Immunol Pract. 2019;7(7):2225-2229 e2221. doi:10.1016/j.jaip.2019.04.021
Garcia Rodriguez R, Moreno Lozano L, Extremera Ortega A, et al. Provocation Tests in Nonimmediate Hypersensitivity Reactions to beta-Lactam Antibiotics in Children: Are Extended Challenges Needed? J Allergy Clin Immunol Pract. 2019 Jan;7(1):265-269.
Mill C, Primeau MN, Medoff E, Lejtenji C, O'Keefe A, Netchiporouk E, et al. Assessing the Diagnostic Properties of a Graded Oral Provocation Challenge for the Diagnosis of Immediate and Nonimmediate Reactions to Amoxicillin in Children. JAMA Pediatr. 2016 Jun 6;170(6):e160033. doi:10.1001/jamapediatrics.2016.0033
De Shryver S NE, Ben-Shoshan M. Severe Serum Sickness-Like Reaction: Challenges in Diagnosis and Management. J Clin Exp Dermatol. Res. 2015 ;6(3):3. doi:10.4172/2155-9554.1000279
Ponvert C, Perrin Y, Bados-Albiero A, et al. Allergy to betalactam antibiotics in children: results of a 20-year study based on clinical history, skin and challenge tests. Pediatr Allergy Immunol. 2011 Jun;22(4):411-418. doi:10.1111/j.1399-3038.2011.01169.x
Iammatteo M, Alvarez Arango S, Ferastraoaru D, et al. Safety and Outcomes of Oral Graded Challenges to Amoxicillin without Prior Skin Testing. J Allergy Clin Immunol Pract. 2019 Jan;7(1):236-243. doi:10.1016/j.jaip.2018.05.008
Kuruvilla M, Shih J, Patel K, Scanlon N. Direct oral amoxicillin challenge without preliminary skin testing in adult patients with allergy and at low risk with reported penicillin allergy. Allergy Asthma Proc. 2019 Jan 1;40(1):57-61. doi:10.2500/aap.2019.40.4184
Stevenson B, Trevenen M, Klinken E, et al. Multicenter Australian Study to Determine Criteria for Low- and High-Risk Penicillin Testing in Outpatients. J Allergy Clin Immunol Pract. 2020 Feb;8(2):681-689 e683. doi:10.1016/j.jaip.2019.09.025
Mustafa SS, Conn K, Ramsey A. Comparing Direct Challenge to Penicillin Skin Testing for the Outpatient Evaluation of Penicillin Allergy: A Randomized Controlled Trial. J Allergy Clin Immunol Pract. 2019 Sep-Oct;7(7):2163-2170. doi:10.1016/j.jaip.2019.05.037
Trubiano JA, Vogrin S, Chua KYL, Bourke J, Yun J, Douglas A, et al. Development and Validation of a Penicillin Allergy Clinical Decision Rule. JAMA Intern Med. 2020 May 1;180(5):745-752. doi:10.1001/jamainternmed.2020.0403
Baldo BA, Pham NH, Weiner J. Detection and side-chain specificity of IgE antibodies to flucloxacillin in allergic subjects. J Mol Recognit. 1995 May-Jun;8(3):171-177. doi:10.1002/jmr.300080302
Blumenthal KG, Peter JG, Trubiano JA, Phillips EJ. Antibiotic allergy. Lancet. 2019 Jan 12;393(10167):183-198. doi:10.1016/S0140-6736(18)32218-9
Ledford DK. Cephalosporin Side Chain Cross-reactivity. J Allergy Clin Immunol Pract. 2015 Nov-Dec;3(6):1006-1007. doi:10.1016/j.jaip.2015.08.014
Zagursky RJ, Pichichero ME. Cross-reactivity in beta-Lactam Allergy. J Allergy Clin Immunol Pract. 2018 Jan-Feb;6(1):72-81 e71. doi:10.1016/j.jaip.2017.08.027