Primary Ciliary Dyskinesia: A Review
DOI:
https://doi.org/10.58931/cait.2021.1323Abstract
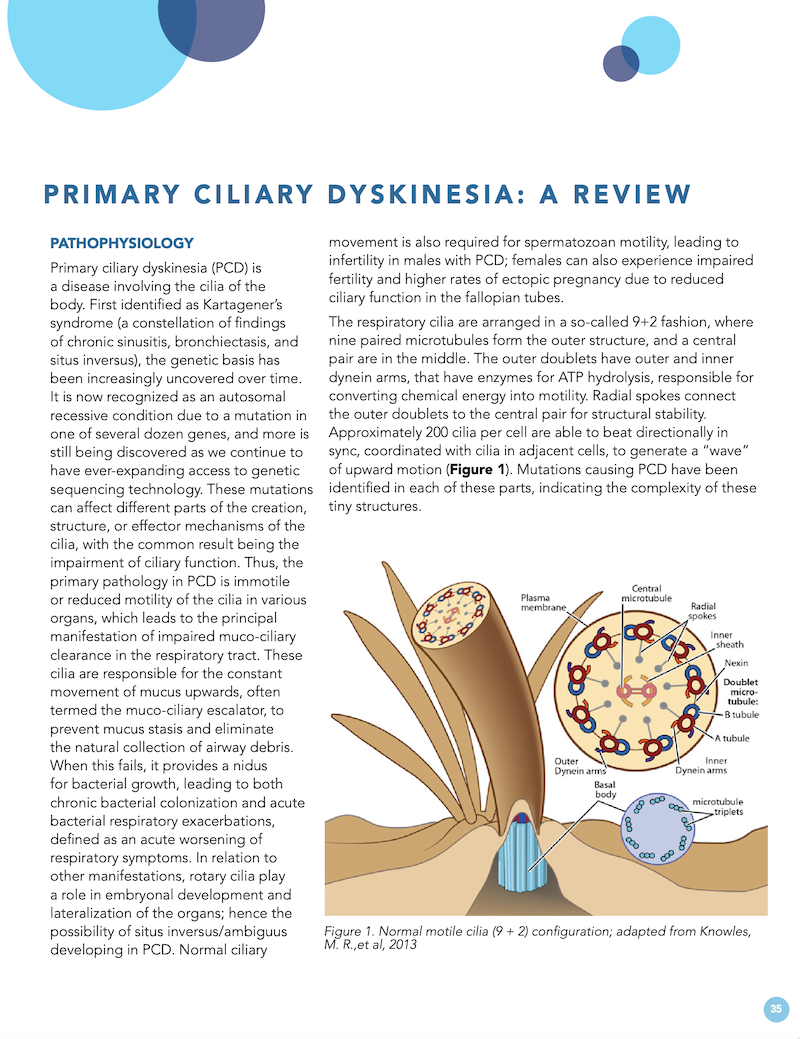
Primary ciliary dyskinesia (PCD) is a disease involving the cilia of the body. First identified as Kartagener’s syndrome (a constellation of findings of chronic sinusitis, bronchiectasis, and situs inversus), the genetic basis has been increasingly uncovered over time. It is now recognized as an autosomal recessive condition due to a mutation in one of several dozen genes, and more is still being discovered as we continue to have ever-expanding access to genetic sequencing technology. These mutations can affect different parts of the creation, structure, or effector mechanisms of the cilia, with the common result being the impairment of ciliary function. Thus, the primary pathology in PCD is immotile or reduced motility of the cilia in various organs, which leads to the principal manifestation of impaired muco-ciliary clearance in the respiratory tract. These cilia are responsible for the constant movement of mucus upwards, often termed the muco-ciliary escalator, to prevent mucus stasis and eliminate the natural collection of airway debris. When this fails, it provides a nidus for bacterial growth, leading to both chronic bacterial colonization and acute bacterial respiratory exacerbations, defined as an acute worsening of respiratory symptoms. In relation to other manifestations, rotary cilia play a role in embryonal development and lateralization of the organs; hence the possibility of situs inversus/ambiguus developing in PCD. Normal ciliary movement is also required for spermatozoan motility, leading to infertility in males with PCD; females can also experience impaired fertility and higher rates of ectopic pregnancy due to reduced ciliary function in the fallopian tubes.
References
Knowles MR, Daniels LA, Davis SD, Zariwala MA, Leigh MW. Primary ciliary dyskinesia. Recent advances in diagnostics, genetics, and characterization of clinical disease. Am J Respir Crit Care Med. 2013 Oct 15;188(8);913-922. doi:10.1164/rccm.201301-0059CI
O’Callaghan C, Chetcuti P, Moya E. High prevalence of primary ciliary dyskinesia in a British Asian population. Arch Dis Child 2010, 95(1):51-52. doi:10.1136/adc.2009.158493
Shapiro AJ, Davis SD, Polineni D, Manion M, Rosenfeld M, Dell SD, et al. Diagnosis of Primary Ciliary Dyskinesia. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2018 Jun 15;197(12), e24-e39. doi:10.1164/rccm.201805-0819ST
Mullowney T, Manson D, Kim R, Stephens D, Shah V, Dell S. Primary ciliary dyskinesia and neonatal respiratory distress. Pediatrics. 2012 Dec;134(6):1160-1166. doi:10.1542/peds.2014-0808
Knowles MR, Daniels LA, Davis SD, Zariwala MA, Leigh MW. Primary ciliary dyskinesia. Recent advances in diagnostics, genetics, and characterization of clinical disease. Am J Respir Crit Care Med 2013;188(8), 913-922. doi:10.1164/rccm.201301-0059CI
Shapir AJ, Davis SD, Polineni D, Manion M, Rosenfeld M, Dell SD, et al. Diagnosis of Primary Ciliary Dyskinesia. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2018 Jun 15;197(12), e24-e39. doi:10.1164/rccm.201805-0819S
Khalid F, Hannah WB, Gaston BM. Rapid Advances in Primary Ciliary Dyskinesia Research. A Brief Update for Pulmonologists. Am J Respir Crit Care Med. 2019 Jan 15;199(2):136-138. doi:10.1164/rccm.201807-1390ED
Goutaki M, Halbeisen FS, Barbato A, Crowley S, Harris A, Hirst RA, Kuehni CE. Late Diagnosis of Infants with PCD and Neonatal Respiratory Distress. J Clin Med. 2020 Sep;9(9):2871. doi:10.3390/jcm9092871
Boon M, Vermeulen FL, Gysemans W, et al. Lung structure-function correlation in patients with primary ciliary dyskinesia. Thorax. 2015 Apr;70(4):339-345. doi:10.1136/thoraxjnl-2014-206578
Marthin JK, Petersen N, Skovgaard LT, Nielsen KG. Lung function in patients with primary ciliary dyskinesia: a cross-sectional and 3-decade longitudinal study. Am J Respir Crit Care Med. 2010;181(11):1262-1268. doi:10.1164/rccm.200811-1731OC