Asthma and Pregnancy: When You Have to Think of Two (Or More) Instead of One
DOI:
https://doi.org/10.58931/cait.2022.2129Abstract
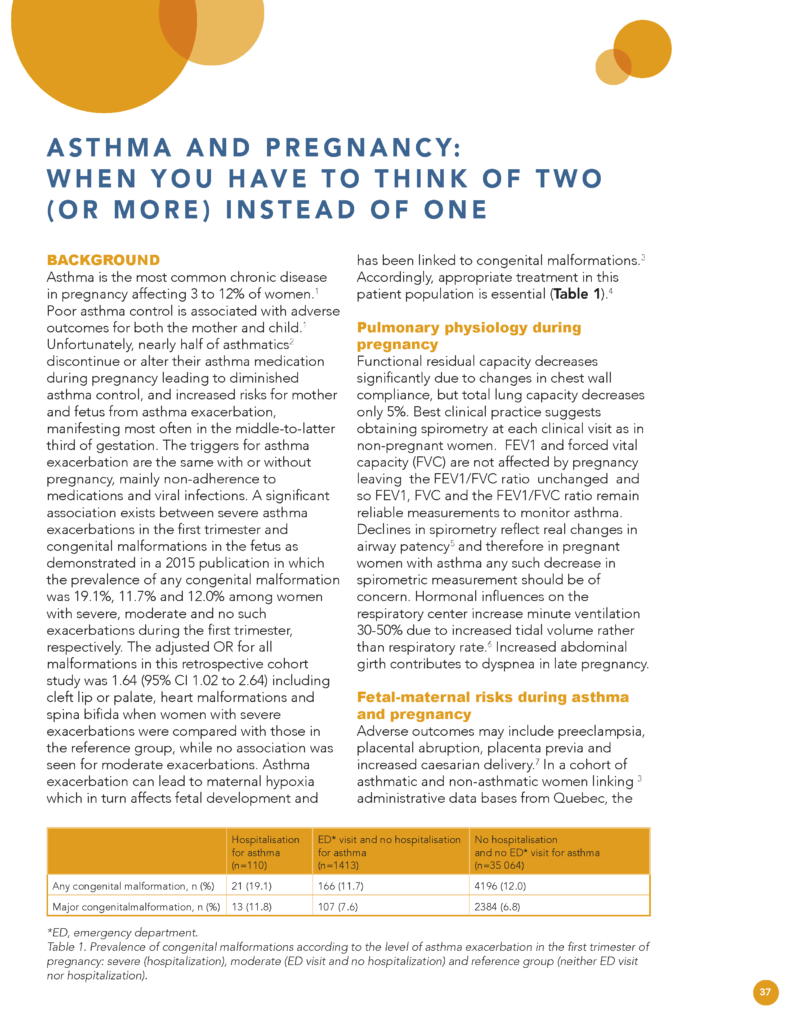
Asthma is the most common chronic disease in pregnancy affecting 3 to 12% of women.Poor asthma control is associated with adverse outcomes for both the mother and child. Unfortunately, nearly half of asthmatics discontinue or alter their asthma medication during pregnancy leading to diminished asthma control, and increased risks for mother and fetus from asthma exacerbation, manifesting most often in the middle-to-latter third of gestation. The triggers for asthma exacerbation are the same with or without pregnancy, mainly non-adherence to medications and viral infections. A significant association exists between severe asthma exacerbations in the first trimester and congenital malformations in the fetus as demonstrated in a 2015 publication in which the prevalence of any congenital malformation was 19.1%, 11.7% and 12.0% among women with severe, moderate and no such exacerbations during the first trimester, respectively. The adjusted OR for all malformations in this retrospective cohort study was 1.64 (95% CI 1.02 to 2.64) including cleft lip or palate, heart malformations and spina bifida when women with severe exacerbations were compared with those in the reference group, while no association was seen for moderate exacerbations. Asthma exacerbation can lead to maternal hypoxia which in turn affects fetal development and has been linked to congenital malformations. Accordingly, appropriate treatment in this patient population is essential.
References
Kwon HL, Belanger K and Bracken MB. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol. 2003;13:317-324.
Enriquez R, Wu P. Griffin MR et al. Cessation of asthma medication in early pregnancy. Am J Obstet Gynecol. 2006;195:149-153.
Webster WS, Abela D. The effect of hypoxia in development. Birth Defects Res C Embryo Today. 2007;81:215-28.
Blais L, Kettani FZ, Forget A et al. Asthma exacerbations during the first trimester of pregnancy and congenital malformations: revisiting the association in a large representative cohort. Thorax. 2015;70:647-52.
Grindheim G, Toska K, Estensen ME, Rossland MA. Changes in pulmonary function during pregnancy: a longitudinal cohort study. BJOG. 2012;119:94-101.
LoMauro A, Aliverti A. Respiratory physiology of pregnancy: physiology masterclass. Breathe. 2015;11(4):297-301.
Mendola P, Laughon SK, Mannisto TI, et al. Obstetric complications among US women with asthma. Am J Obstet Gynecol. 2013;208:127.
Blais l, Kettani FZ, Forget A. Relationship between maternal asthma, its severity and control and abortion. Hum Reprod. 2013;28(4):908-15.
Gade EJ, Thomsen SF, Lindenberg S, et al. Fertility oucomes in asthma: a clinical study of 245 women with unexplained infertility. Eur Respir J. 2016;47:1144-51.
Wang G, Murphy VE, Namazy J, et al. The risk of maternal and placental complications in pregnant women with asthma: a systematic review and meta-analysis. J Matern Fetal Neonat Med. 2014;27:934-942.
Grzeskowski LE, Smith B, Roy A, et al. Patterns, predictors and outcomes of asthma control and exacerbations during pregnancy: a prospective cohort study. ERJ Open Res. 2016;2(1):00054-2015.
Murphy V, Wark PA, Gibson PG. A prospective study of respiratory viral infection in pregnant women with and without asthma. Chest. 2013;144:420-7.
Meijer WJ, van Noortwijk AG, Bruinse HW, Wensing AM. Influenza viral infection in pregnancy: a review. Acta Obstet Gynecol Scand. 2015;94:797-819.
Powell H, Murphy VE, Hensley MJ, et al. Rhinitis in pregnant women with asthma is associated with poorer asthma control and quality of life. J Asthma. 2015;52:1023-30.
Bidad K, Heidernazhadh, Pourpak Z, et al. Gastroesophageal reflux and asthma in pregnant women with dyspnea. Iran J Asthma Allergy Immunol. 2014;13:104-109.
Xia-Hong C, Yu-Peng X, Xiu-Cui L, et al. The prevalence and associated risk factors of sleep disorder-related symptoms in pregnant women in China. Sleep Breath. 2013;17:951-6.
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2020 Jun.
Shakespeare J, Tuffnell D, Kurinczuk J, et al., eds. Saving lives, improving mothers care-lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2013-2015. Maternal, Newborn and Infant Clinical Outcome Review Programme. 2017 Nov.
Cox L, Nelson H, Lockey R et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol. 2011;127:S1-S55.
Abdallah K, Zhu J, Gershon A, et al. Effect of asthma exacerbation during pregnancy in women with asthma; a population-based cohort study. Eur Respir. 2020;55:19013305.
Garne E, Vinken HA, Morris J, et al. Risk of congenital anomalies after exposure to asthma medication in the first trimester of pregnancy – a cohort linkage study. BJOG. 2016;123:1609-18.
Blais L, Beauchesne MF, Lemiere C, et al. High doses of inhaled corticosteroids during the first trimester of pregnancy and congenital malformations. J Allergy Clin Immunol. 2009;124:1229-1234.
Cossette B, Forget A, Beachesne MF, et al. Impact of use of asthma-controller therapy on perinatal outcomes. Thorax. 2013;68(8):724-730.
Wang H, Li Na, Huang H. Asthma in pregnancy: pathophysiology, diagnosis, whole-course management, and medication safety. Can Respir J. 2020;9046842.
SIGN-BTS. Sign 158. British guideline on the management of asthma. Health Improvement Scotland, British Thoracic Society. July 2019.
Cossette B, Forget A, Beauchesne MF, et al. Impact of maternal asthma-controller therapy on perinatal outcomes. Thorax. 2013;68:724-730.
Yang CL, Hicks EA, Mitchell P, et al. 2021 Canadian Thoracic Society Guidelines-a focused update on the management of very mild and mild asthma. Can J Respir Crit Care Sleep Med. 2021 Feb;5(4):205-245.
O Byrne P, Fitzgerald JM, Bateman ED, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N Engl J Med. 2018;378:1865-1876.
Weinberger E, Schatz M. Management of asthma during pregnancy. UpToDate. 2020.
NAEPP expert panel report. Managing asthma during pregnancy: recommendations for pharmacologic treatment-2004 update. J Allergy Clin Immunol. 2005;115:34-46 doi:10.1016/j.jaci.2004.10.023
Palmeira P, Quinello C, Silveira-Lessa AL, et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012:985646.
Namazy J, Cabana MD, Scheuerle AE, et al. The Xolair Pregnancy Registry (EXPECT): the safety of omalizumab use during pregnancy. J Allergy Clin Immunol. 2015;135(2):407-412.
Bonham CA, Patterson KC, Strek ME. Asthma Outcomes and management during pregnancy. Chest. 2018 Feb;153(2)515-27.
US Food and Drug Administration (FDA). Highlights of prescribing information: Nucala (mepolizumab), 2015; US Food and Drug Administration (FDA). Highlights of prescribing information: Fasenra (benralizumab) 2017.
Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measure of fraction exhaled nitric oxide: a double-blind, andomized control trial. Lancet. 2011;378:983-990.
Girling J. Prescribing for pregnancy: asthma. Drug Ther Bull. 2020;58:41-44.
Couillard S, Connolly C, Borg C, Pavord I. Asthma in pregnancy: An update. Obstetric Medicine. 2021;14(3):135-144.
Juniper EF, O’Byrne PM, Guyatt GH, et al. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14:902-7.