Emerging Biologics in the Management of Atopic Dermatitis
DOI:
https://doi.org/10.58931/cait.2025.5177Abstract
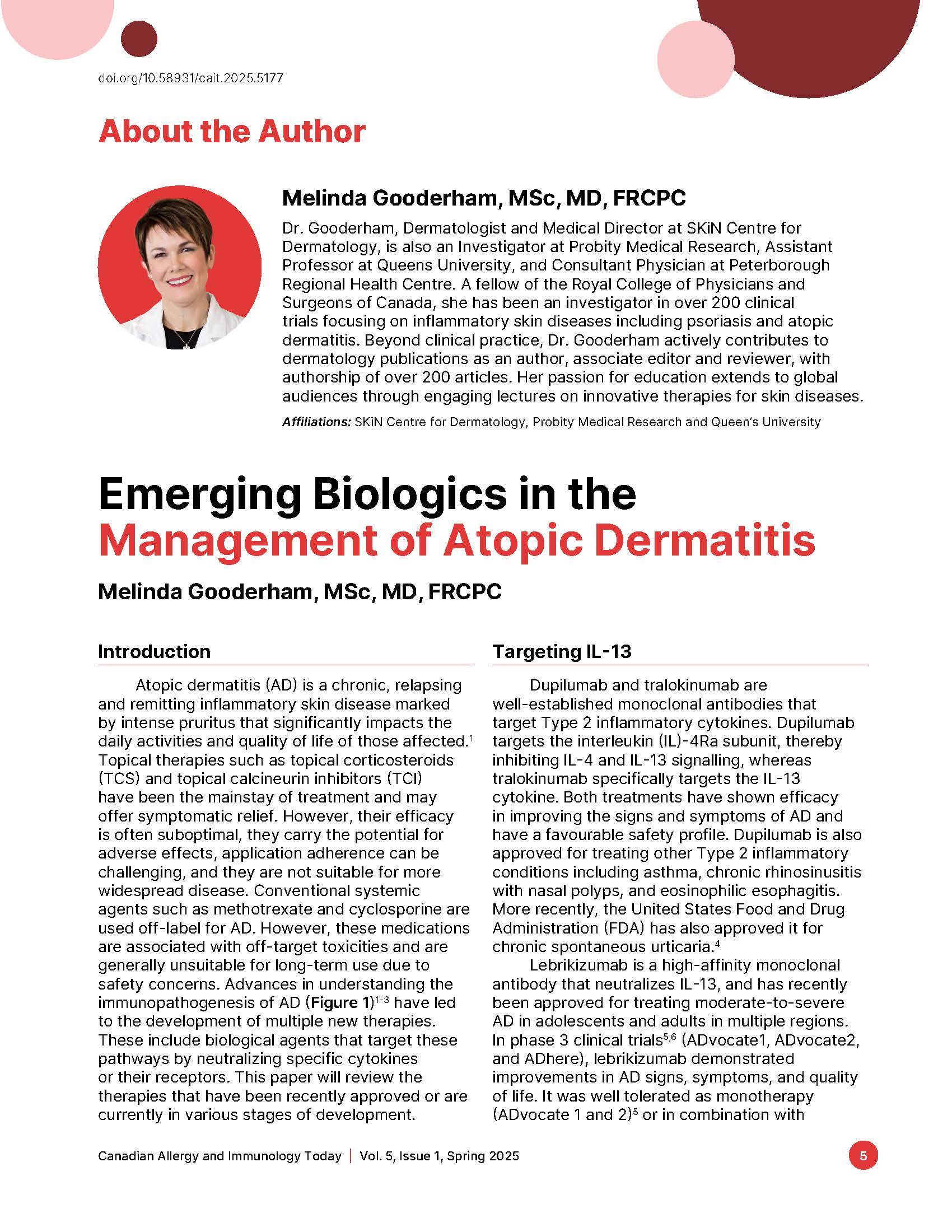
Atopic dermatitis (AD) is a chronic, relapsing and remitting inflammatory skin disease marked by intense pruritus that significantly impacts the daily activities and quality of life of those affected. Topical therapies such as topical corticosteroids (TCS) and topical calcineurin inhibitors (TCI) have been the mainstay of treatment and may offer symptomatic relief. However, their efficacy is often suboptimal, they carry the potential for adverse effects, application adherence can be challenging, and they are not suitable for more widespread disease. Conventional systemic agents such as methotrexate and cyclosporine are used off-label for AD. However, these medications are associated with off-target toxicities and are generally unsuitable for long-term use due to safety concerns. Advances in understanding the immunopathogenesis of AD (Figure 1) have led to the development of multiple new therapies. These include biological agents that target these pathways by neutralizing specific cytokines or their receptors. This paper will review the therapies that have been recently approved or are currently in various stages of development.
References
Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. 2018;4(1):1. doi:10.1038/s41572-018-0001
Facheris P, Jeffery J, Del Duca E, Guttman-Yassky E. The translational revolution in atopic dermatitis: the paradigm shift from pathogenesis to treatment. Cell Mol Immunol. 2023;20(5):448-474. doi:10.1038/s41423-023-00992-4
Huang I-H, Chung W-H, Wu P-C, Chen C-B. JAK–STAT signaling pathway in the pathogenesis of atopic dermatitis: an updated review. Front Immunol. 2022;13:1068260. doi:10.3389/fimmu.2022.1068260
Sanofi. Press Release: Dupixent late-breaking positive phase 3 data in chronic spontaneous urticaria to be presented at ACAAI [Internet]. Paris: Sanofi; 2024 Oct 24 [cited 2025 May 3]. Available from: https://www.sanofi.com/en/media-room/press-releases/2024/2024-10-24-12-00-00-2968628
Silverberg JI, Guttman-Yassky E, Thaçi D, Irvine AD, Stein Gold L, Blauvelt A, et al. Two phase 3 trials of lebrikizumab for moderate-to-severe atopic dermatitis. N Engl J Med. 2023;388(12):1080-1091. doi: 10.1056/NEJMoa2206714.
Simpson EL, Gooderham M, Wollenberg A, Weidinger S, Armstrong A, Soung J, et al. Efficacy and safety of lebrikizumab in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis: a randomized clinical trial (ADhere). JAMA Dermatol. 2023;159(2):182-191. doi:10.1001/jamadermatol.2022.5534
Silverberg JI, Wollenberg A, Reich A, Thaci D, Legat FJ, Papp KA, et al. Nemolizumab with concomitant topical therapy in adolescents and adults with moderate-to-severe atopic dermatitis (ARCADIA 1 and ARCADIA 2): results from two replicate, double-blind, randomised controlled phase 3 trials. Lancet. 2024;404(10451):445-460. doi:10.1016/S0140-6736(24)01203-0
Sadrolashrafi K, Guo L, Kikuchi R, Hao A, Yamamoto RK, Tolson HC, et al. An OX-Tra’Ordinary tale: the role of OX40 and OX40L in atopic dermatitis. Cells 2024;13(7):587. doi:10.3390/cells13070587
Weidinger S, Blauvelt A, Papp KA, Reich A, Lee C-H, Worm M, et al.. Phase 2b randomized clinical trial of amlitelimab, an anti-OX40 ligand antibody, in patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol. 2025;155(4):1264-1275. doi:10.1016/j.jaci.2024.10.031
Guttman-Yassky E, Simpson E, Bissonnette R, Eichenfield LF, Kabashima K, Luna PC, et al. ROCKET: a phase 3 program evaluating the efficacy and safety of rocatinlimab in moderate-to-severe atopic dermatitis. Immunotherapy. 2025;17(2), 83-94. doi:10.1080/1750743X.2025.2464528
Guttman-Yassky E, Simpson EL, Reich K, Kabashima K, Igawa K, Suzuki T, et al. An anti-OX40 antibody to treat moderate-to-severe atopic dermatitis: a multicentre, double-blind, placebo-controlled phase 2b study. Lancet. 2023;401(10372):204-214. doi:10.1016/S0140-6736(22)02037-2
Gooderham M, Guttman-Yassky E, Igawa K, Kabashima K, Esfandiari E, Rylands AJ, et al. Rocatinlimab improves patient-reported outcomes in adults with moderate-to-severe atopic dermatitis: results from a double-blind placebo-controlled phase 2b study. Dermatol Ther (Heidelb). 2024;14:3351-3366. doi:10.1007/s13555-024-01303-z
Guttman-Yassky E, Brunner PM, Neumann AU, Khattri S, Pavel AB, Malik K, et al. Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: a randomized, double-blind, phase 2a trial. J Am Acad Dermatol. 2018;78(5):872-881.e6. doi:10.1016/j.jaad.2018.01.016
Gooderham M, Reich A, Laquer V, Lynde C, Soong W, Worm M, et al. 53111 Individual patient responses to IL-22RA1 inhibition in a phase 2a monotherapy trial for moderate-to-severe atopic dermatitis. Journal of the American Academy of Dermatology. 2024; 91(3), AB239. https://doi.org/10.1016/j.jaad.2024.07.951
Nakajima S, Kabata H, Kabashima K, Asano K. Anti-TSLP antibodies: targeting a master regulator of type 2 immune responses. Allergol Int. 2020;69(2):197-203. doi:10.1016/j.alit.2020.01.001
Simpson EL, Parnes JR, She D, Crouch S, Rees W, Mo M, et al. Tezepelumab, an anti–thymic stromal lymphopoietin monoclonal antibody, in the treatment of moderate to severe atopic dermatitis: a randomized phase 2a clinical trial. J Am Acad Dermatol. 2019;80(4):1013-1021. doi:10.1016/j.jaad.2018.11.059
Maurer M, Cheung DS, Theess W, Yang Y, Dolton M, Guttman A, et al. Phase 2 randomized clinical trial of astegolimab in patients with moderate to severe atopic dermatitis. J Allergy Clin Immunol. 2022;150(6):1517-1524. doi:10.1016/j.jaci.2022.08.015
ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US); Efficacy, safety, and pharmacokinetic profile of etokimab (ANB020) in Adult participants with moderate-to-severe atopic dermatitis (ATLAS); [updated 2023 May 24, cited 2025 May 4]; Report No.: NCT03533751. Available from: https://clinicaltrials.gov/study/NCT03533751
Alvarenga JM, Bieber T, Torres T. Emerging biologic therapies for the treatment of atopic dermatitis. Drugs. 2024;84(11):1379-1394 doi:10.1007/s40265-024-02095-4
Yilmaz O, Torres T. Extended half-life antibodies: a narrative review of a new approach in the management of atopic dermatitis. Dermatol Ther (Heidelb). 2024;14(9):2393-2406. doi:10.1007/s13555-024-01253-6